For hospitals, it is 4x harder to collect from patients than insurance payers. Patients now make up to 30% of hospital revenue but are 4x harder to collect from than insurance payers1 due to complexity, regulation and patient means.
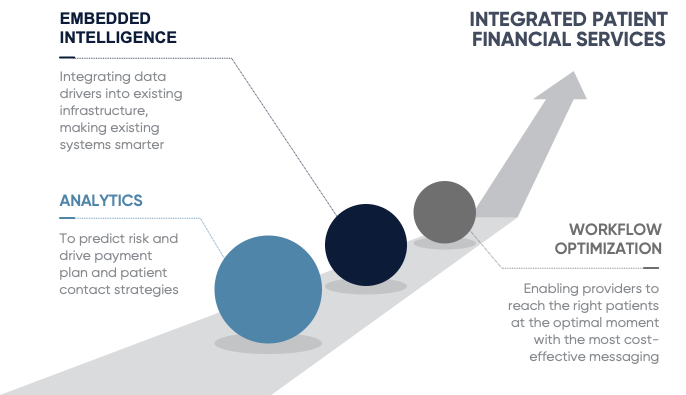
Sift Healthcare provides advanced analytics and machine learning integrations to optimize patient payments. Sift combines patient payment expertise and AI-driven intelligence to equip providers with an integrated toolset to optimize patient financial engagement.
Patient collections should be a dialogue, not a solicitation. Sift integrates AI into your patient engagement platform to guide patient communications activities – maximizing collections while improving patient engagement.
- Account Segmentation
- Patient Contact Strategy
- Payment Plan Provisioning
- Improved collections, increased payment plan adoption, and reduced inbound/outbound calls
Propensity-to-pay for a person, not a number. Sift goes beyond credit scores, leveraging historical data to determine the best engagement approach for each patient.
- Improved Patient Satisfaction
- Pre-service patient financing and collection recommendations that help avoid surprises and set expectations
- Lookalike predictive models, not credit scores and rule logic
- Increased upfront collections with more empathy