CONTINUALLY INNOVATING TO MEET INDUSTRY NEEDS
Addressing Electronic Prior Authorization for Drugs Under the Medical Benefit
With an influx of infused medications being administered in physician offices, prior authorizations for drugs billed under the medical benefit are presenting challenges across the industry. While there is an industry NCPDP SCRIPT standard for electronic prior authorization (ePA) for drugs billed under the pharmacy benefit, driving significant ePA volume, an industry standard does not currently exist for drugs under the medical benefit.
The challenge with adopting the NCPDP SCRIPT standard for drugs under the medical benefit is that these medications typically do not go the standard route of provider e-prescribing to a traditional retail or mail-order pharmacy location. Often times, the specialty medications are being purchased by the provider (physician/infusion center) directly from drug distributors and administered in the office setting. As a result, health plans continue to receive the drugs under the medical benefit prior authorization requests via phone, fax, or portal which is placing an enormous administrative burden on the health plans operations team, provider office, and the patient.
Agadia continues to innovate and has addressed these challenges by providing eMPA capabilities to reduce the prior authorization administrative burden through a more efficient channel that increases automation and improves turnaround times. Providers will benefit by quickly being informed whether the drug is under the pharmacy or medical benefit, allowing them to efficiently manage requests. Hub companies will experience improved efficiencies as well such as faster turnaround times for a prior authorization decision, improved patient speed to therapy and better adherence.
LEVERAGE ADVANCED TECHNOLOGIES
Save Valuable Time & Resources with PAHub’s Auto-Decision
PAHub’s Auto-Decision rules engine increases automation be leveraging data mining techniques across enterprise systems data to electronically adjudicate prior authorization requests. Auto-Decision helps a customer to allocate staff to high-touch requests instead of requests that can be adjudicated automatically.
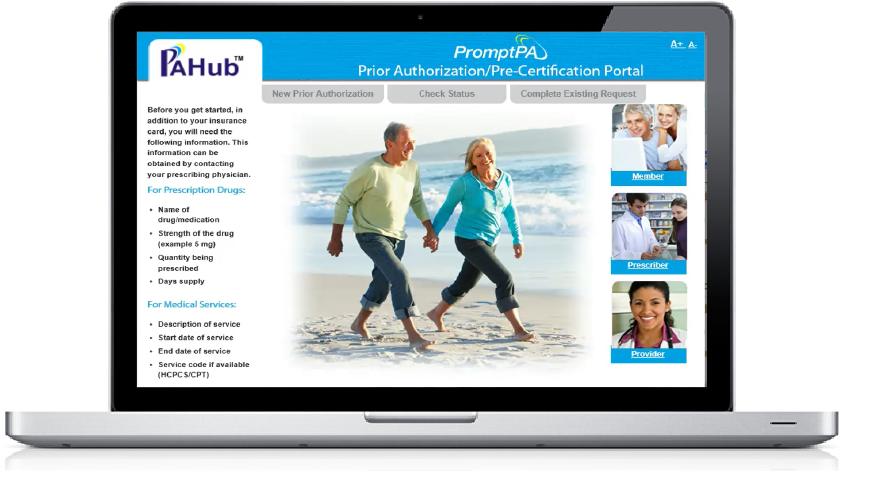
ENGAGE PHARMACIES, MEMBERS & PROVIDERS
In the Prior Authorization and Pre-Certification Process
PromptPA is a self-service, web based solution that enables our customers’ pharmacies, members and providers to request prior authorizations electronically, initiate renewals and check the status of requests using any web browser, reducing operational costs and call volume to Health Plans and Benefit Managers.