Administrative Cost Savings
eviCore’s medical benefits management solutions are proven to reduce unnecessary–and potentially harmful–tests and procedures. But securing prior authorization can impose a high burden on provider organizations; for example, dedicated administrative staff are hired to request and track cases, and clinicians typically must allocate time to provide details on the patient’s medical diagnosis.
In place of implementing an abundance of tools, multiple health plan portals, and time-consuming manual interactions, eviCore intelliPath® simplifies and streamlines prior authorization operations with a single, integrated application. eviCore intelliPath® leverages the substantial investment in EMRs on the part of provider networks. It automatically incorporates case details from the patient’s chart and fits seamlessly into clinical and revenue cycle workflows.
Clinical Efficiency
Further, eviCore intelliPath® integrates with eviCore’s utilization management system (and those of other UM providers). This speeds communication of critical information (e.g., automated approval, no prior authorization required, or additional clinical information is needed for a decision to be made). With the approval or denial in hand, patients can be scheduled or alternative tests or procedures ordered in a timely fashion.
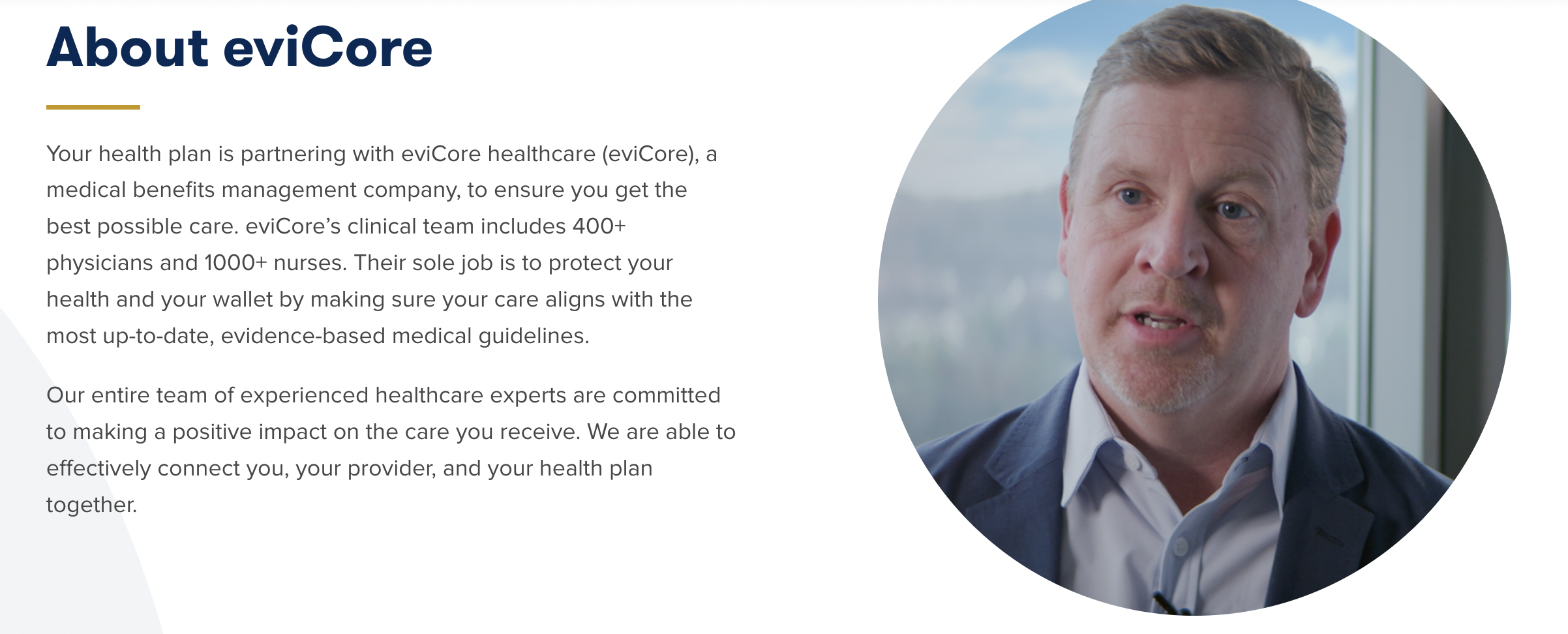
Benefits for Patients, Providers, and Health Plans
- Lower costs for healthcare-delivery organizations
- Reduced frustration and more transparency for patients and clinicians
- Better network relationships for health plans