OnCare360 stands out with its comprehensive, integrated platform designed to streamline workflows and improve patient outcomes:
1. All-in-One Platform: Combines tools for RPM, CCM, TCM, PCM, AWV, SDOH, ACP, and more, eliminating the need for multiple systems.
2. Program-Specific Features: Tailored workflows, care plan templates, and automated time tracking for each CMS program ensure ease of implementation and compliance.
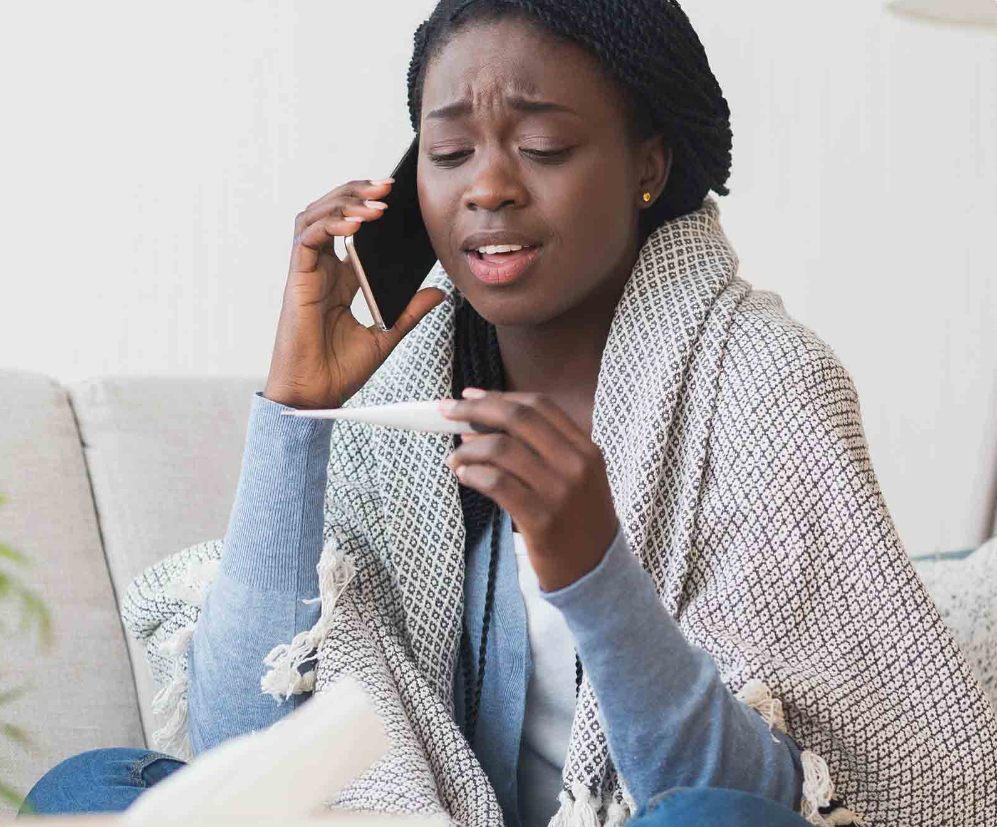
3. Patient Engagement Tools: Secure portals, reminders, and educational resources promote adherence and satisfaction, surpassing basic communication solutions offered by competitors.
4. Compliance Automation: Preloaded CPT codes, billing accuracy checks, and audit-ready documentation reduce errors and maximize reimbursements.
5. SDOH and Holistic Care: Advanced tools to assess and address non-medical factors, linking patients to resources and improving health equity.
6. Scalability and Flexibility: Suitable for small practices, large health systems, and ACOs, with customizable workflows for diverse needs.
7. Real-Time Insights: Analytics dashboards provide actionable data on care outcomes, performance metrics, and patient risks.
OnCare360 delivers unmatched versatility, compliance, and patient engagement features.