1. Care Gap Closure & Population Health
Automatically identifies patients who are overdue for preventive services (screenings, vaccines, chronic care visits) and guides outreach and follow-up—helping improve quality scores, avoid penalties, and meet value-based care targets.
2. Prior Authorization & Denial Management
Uses AI agents to automate the entire prior-auth lifecycle—from intake and documentation to status tracking and appeals—reducing delays, administrative cost, and claim denials.
3. Medicaid Re-determination & Uncompensated Care Reduction
Flags patients at risk of losing coverage, assists them through re-enrollment, and minimizes lapses that drive bad debt or charity care—directly protecting revenue.
4. Referral Management & Network Leakage Prevention
Optimizes specialist referrals and ensures patients stay within network, improving continuity of care and capturing downstream revenue.
5. Scheduling & Capacity Optimization
Analyzes real-time demand and provider availability to maximize clinic and inpatient throughput, cut no-shows, and improve staff utilization.
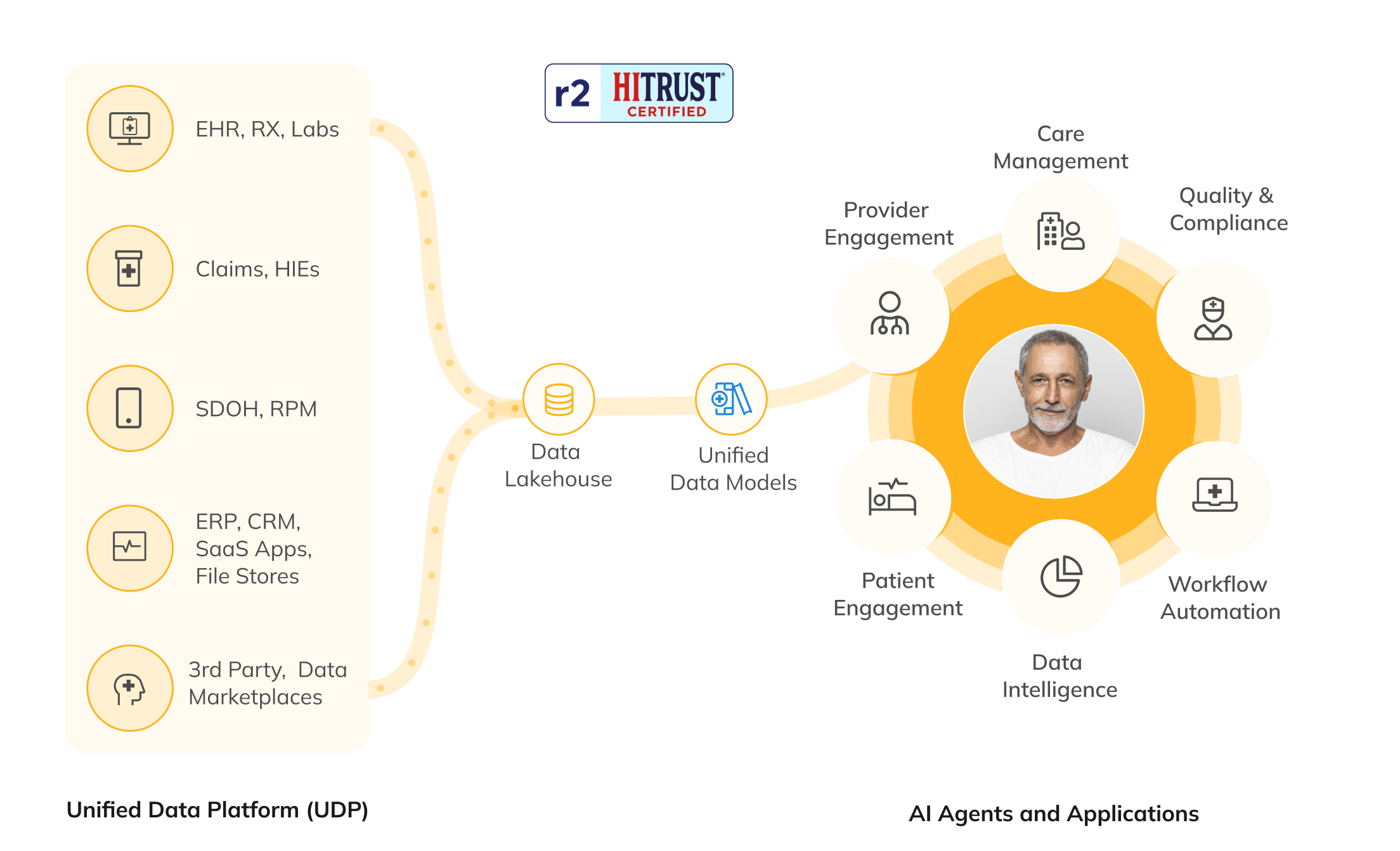
6. AI-Driven Clinical & Operational Command Center
Unifies data across 50+ systems and layers predictive/agentic AI for service-line performance, quality reporting, and population risk insights—empowering leaders with a single source of truth for strategic decisions.